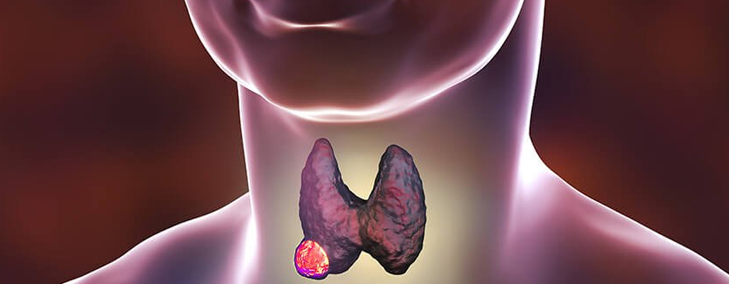
What Is the Thyroid Gland?
The thyroid is a gland in the base of the neck, near the windpipe. It is shaped like a butterfly, with a right lobe and a left lobe. A healthy thyroid is around 4 cm in size. It usually cannot be felt through the skin. The thyroid uses iodine, a mineral found in some foods and in iodized salt, to help make several hormones. Thyroid hormones affect every cell and all the organs of the body. They regulate the rate at which calories are burned, affecting weight loss or weight gain. Can slow down or speed up the heartbeat, affect the digestive system and the nervous system.
What Are the Common Diseases of the Thyroid Gland?
Common thyroid diseases can be classified into these:
- Hyperthyroidism: a group of disorders in which the thyroid gland produces more hormone than it usually does.
- Hypothyroidism: a group of disorders in which thyroid gland produces less hormone then it usually does.
- Nodular thyroid disease: various disorders associated with the presence of nodules in the thyroid gland
- Thyroid cancer
- Other miscellaneous thyroid disorders
What Is a Thyroid Nodule?
Any abnormal growth in the thyroid gland is known as a thyroid nodule. It is important to note that most thyroid nodules are not cancer.
When a thyroid nodule is found, an ultrasound of the thyroid and a fine-needle aspiration biopsy are often done to check for signs of cancer. Blood tests to check thyroid hormone levels and for antithyroid antibodies in the blood may also be done to check for other types of thyroid disease.
Thyroid nodules usually don’t cause symptoms or need treatment.
What Is Thyroid Cancer?
Thyroid cancer is a disease in which some cells of the thyroid gland begin to grow uncontrollably and destroy body tissue. The cancer may later also spread to other parts of the body.
Signs of Thyroid Cancer:
Thyroid cancer may not cause early signs or symptoms. It is sometimes found during a routine physical exam. Signs or symptoms may occur as the tumour gets bigger. Other conditions may cause the same signs or symptoms. Check with your doctor if you have any of the following:
- A lump (nodule) in the neck.
- Trouble breathing.
- Trouble swallowing.
- TPain when swallowing.
- Hoarseness.
Tests that examine the thyroid, neck, and blood are used to diagnose thyroid cancer.
There are different types of thyroid cancer.
Thyroid cancer can be described as either:
- Differentiated thyroid cancer, which includes well-differentiated tumors (commonly papillary and follicular),
- Poorly differentiated tumors
- Undifferentiated (Anaplastic) tumors
- Medullary thyroid cancer.
Well-differentiated tumors (papillary thyroid cancer and follicular thyroid cancer) can be treated and can usually be cured.
Poorly differentiated and undifferentiated tumors (anaplastic thyroid cancer) are less common. These tumors grow and spread quickly and have a poorer chance of recovery.
Medullary thyroid cancer is a neuroendocrine tumor that develops in C cells of the thyroid. The C cells make a hormone (calcitonin) that helps maintain a healthy level of calcium in the blood.
Factors affecting chance of having and treatment of thyroid cancer
Age, gender, and being exposed to radiation can affect the risk of thyroid cancer.
What to Expect After a Diagnosis of Thyroid Cancer?
After thyroid cancer has been diagnosed, tests are done to find out if cancer cells have spread within the thyroid or to other parts of the body.
The process used to find out if cancer has spread within the thyroid or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the patient’s age and the stage of the cancer to plan treatment.
Besides these treatments, few other treatments are also under research for the treatment of thyroid cancer.
In selected patients, no active treatment may be undertaken with the patient put under close follow up. (Watchful waiting)
Treatment for thyroid cancer may cause side effects.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Follow-up tests may be needed.
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests. Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment of Stages I, II, and III Papillary and Follicular Thyroid Cancer (Localized/Regional)
Treatment of stage I (younger than 55 years; 55 years and older), stage II (younger than 55 years; 55 years and older), and stage III papillary and follicular thyroid cancer may include the following:
- Surgery (thyroidectomy or lobectomy).
- Radioactive iodine therapy.
- Hormone therapy to prevent the body from making thyroid-stimulating hormone (TSH).
- External radiation therapy.
Treatment of Stage Iv Papillary and Follicular Thyroid Cancer (Metastatic)
When cancer has spread to other places in the body, such as the lungs and bone, treatment usually does not cure the cancer, but can relieve symptoms and improve the quality of life. Treatment of stage IV papillary and follicular thyroid cancer may include the following:
Treatment of Recurrent Papillary and Follicular Thyroid Cancer
Treatment of recurrent papillary and follicular thyroid cancer may include the following:
- Surgery to remove the tumor with or without radioactive iodine therapy.
- Radioactive iodine therapy when the cancer can be found only by a thyroid scan and cannot be felt during a physical exam.
- Targeted therapy with a tyrosine kinase inhibitor (sorafenib, lenvatinib, selpercatinib, larotrectinib, or entrectinib)
- External radiation therapy or intraoperative radiation therapy as palliative therapy to relieve symptoms and improve the quality of life.
- Chemotherapy.
Treatment of Medullary Thyroid Cancer
For information about the treatments listed below, see the Treatment Option Overview section. Localized medullary thyroid cancer is in the thyroid only and may have spread to nearby muscles in the neck. Locally advanced and metastatic thyroid cancer has spread to other parts of the neck or to other parts of the body.
Treatment of Anaplastic Thyroid Cancer
Treatment of anaplastic thyroid cancer may include the following:
- Total thyroidectomy as palliative therapy to relieve symptoms and improve the quality of life for patients whose cancer is in or near the thyroid.
- Tracheostomy as palliative therapy to relieve symptoms and improve the quality of life.
- External radiation therapy..
- Chemotherapy.
- Targeted therapy with protein kinase inhibitors (dabrafenib and trametinib) for patients with a certain mutation in the BRAF gene.